Sahar started her career as a clinical pharmacist and now is a successful CEO of NeuroPharm. She is board certified, an advanced fellow in anti-aging and regenerative medicine and an internationally known speaker in the areas of pain management and bio-identical hormone replacement therapy (BHRT), authoring several books, articles and patient education material in the area of pain management and functional medicine.
Stay tuned for Sahar’s upcoming book entitled Metabolic Approach to Pain Management-Opioid Free.
Sahar’s Expertise Offerings
Personal Consultations
Real health starts with a health care provider who cares. We will discuss your health and tailor my recommendations to your unique needs.
Education
Watch my presentations to some of the industry leaders in integrative medicine. You can also review my professional publications to see how they may apply to you or your patients.
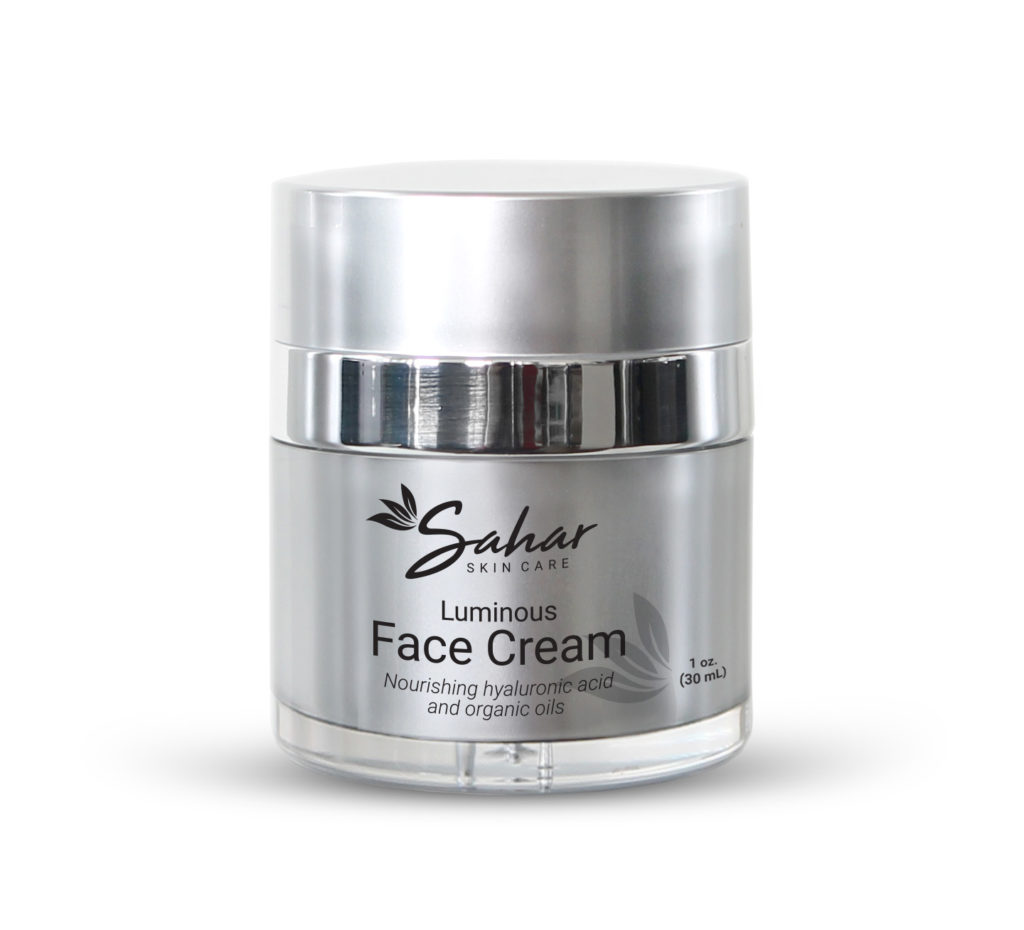
Sahar Skin Care
Professional skin care line developed using scientific evidence, innovative ingredients, and clinical experience to refresh, restore, and awaken your skin's full cellular potential.

Sahar's Preferred
Supplements
When considering nutritional supplements, only consider the best pharmaceutical grade supplements. Shop my store to purchase the products I recommend for optimal health.
Dr. Sahar Swidan is a proud supporter of the LDN Research Trust. Please watch this important documentary about Low Dose Naltrexone (LDN). This innovative therapy could potentially help people who are suffering from chronic pain and other autoimmune disorders. This is a unique treatment available world wide and has changed the lives of millions across the globe.
Click here to watch Dr. Sahar Swidan - 2nd May 2018
from LDN Research Trust on Vimeo.

Highest Quality Pharmaceutical Grade Supplements Available
Quality of supplements is critical for optimal health outcomes. Supplements are powerful tools that we can use to complement an integrative medicine approach to optimal well-being. With Sahar’s extensive knowledge and experience in pharmaceuticals and nutritional supplements, she will guide you along the path to optimal individualized care with quality products.
Sahar’s dedication to helping others achieve their ideal beauty, paired with her extensive pharmaceutical and nutraceutical knowledge, brings to life her premier skin care line. Created on a foundation of health, happiness, and well-being, Sahar’s products will refresh, restore, and awaken your skin.

Refresh
Restore
Awaken
TRUSTED PHARMACIST AND EDUCATOR

Sahar has presented clinical knowledge on a variety of topics at many national and international medical conferences and symposia. Her extensive knowledge in a variety of medical topics with focus on pain management, neurology, headaches and hormone replacement therapy makes her a perfect speaker at your next educational event.